Background & Significance: In current recommendations, consolidative autologous stem cell transplant (ASCT) is essential in management of NDMM. The IFM 2009 Trial showed that RVd followed by ASCT with 1-year lenalidomide maintenance was associated with a better PFS vs. RVd with 1-year lenalidomide maintenance alone (Attal M et al, NEJM 2017). A longer follow up (8 years) of IFM trial concluded that a delayed transplant (in 2 nd line) had no impact on the PFS2 (Perrot A et al, Blood 2020). We evaluated the merit of frontline ASCT (CR1) vs. post salvage ASCT (CR2) in light of indefinite maintenance therapy post novel triplet/quadruplet induction.
Material & Methods: We conducted this retrospective analysis, of symptomatic myeloma patients who underwent ASCT at Rajiv Gandhi Cancer Centre, Delhi between April 2017 and October 2022. Patients were segregated into 2 cohorts; a) ASCT CR1- who received 4 to 6 cycles of RVd (+/- Anti CD38 antibody) induction followed by transplant and indefinite maintenance and b) ASCT CR2- patients who relapsed after 4-6 cycles of RVd induction+maintenance then salvaged with 2 to 6 cycles of novel agent-based therapy (Carfilzomib/ Pomalidomide/ Daratumumab) followed by ASCT and indefinite maintenance. Patient characteristics were balanced for age, gender, ISS, RISS and high risk cytogenetics (Del p53, t(4;14), t (14;16), 1qGain, 1pDel, 13qDel). Response was assessed as per IMWG criteria. PFS was defined as the time from induction/salvage to progression on next line of therapy or death.
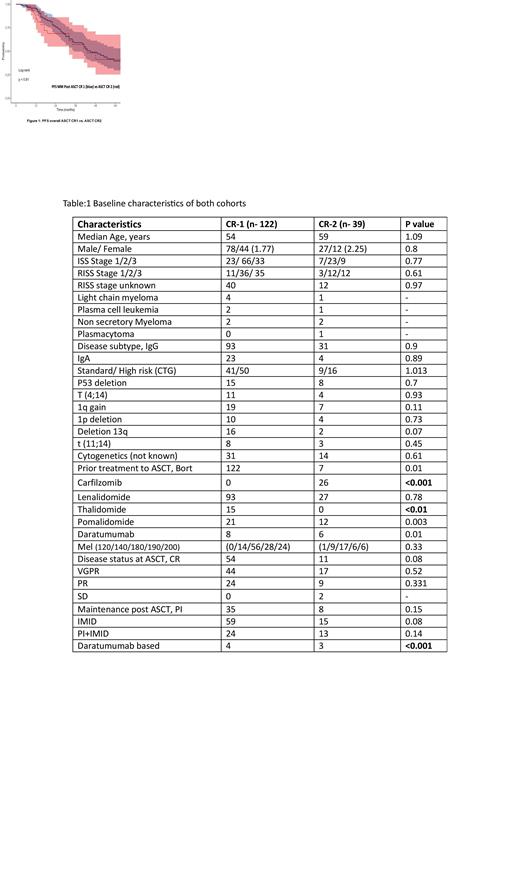
Results: Of 161 patients included, we compared outcomes of ASCT CR 1 (N=122) to ASCT CR-2 (N=39). All patients received maintenance (PI/IMID or in combination) post ASCT. Significant patients in ASCT-CR2 received novel salvage therapy (Carfilzomib/ Pomalidomide/ Daratumumab) (CR1-14 % vs CR2-100%, p value- <0.01). 86% patients in ASCT CR1 received RVd. Both groups were substantially exposed to Lenalidomide. Median time from diagnosis to transplant was 5.9 months (range 4-12) in ASCT- CR1 group and 29.5 months (range 18-64) in ASCT CR2 group (p value- 0.004). After a median follow up of 44 months for ASCT CR1 vs. ASCT CR2, the ORR (97% vs. 95.4%, p=0.88) and CR (85% vs. 78%, p=0.67), respectively. 42.6% patients in ASCT CR1 and 38.4% patients in ASCT CR2 relapsed (p value- 0.4%). The median PFS for both groups (ASCT CR1 and ASCT CR2) were similar 45 months and 43 months, respectively, (p value- 1.09). The 1-, 3- and 5-year PFS showed a similar trend across cohorts (CR-1: 95%, 59.1%, 39.7% and CR-2: 84%, 57.1%, 41.3%). Patients with high-risk cytogenetics in ASCT CR 1 (N=50) had a better median PFS (25 months) compared to ASCT CR2 (N=16, median PFS=17.9 months, p=0.059), fig:1 though statistically insignificant. Table:1 No difference in PFS for standard risk noted (p=0.38). On regression analysis, factors predictive of progression were: ISS stage III (univariate only), high-risk cytogenetics, IMID based maintenance therapy. We noted better PFS in patients receiving >24 months of maintenance. Depth of response prior to transplant, Melphalan dosage and remission (CR1 vs CR2) did not predict progression.
Conclusion: In the light of above findings, does transplant decision need re-sequencing? Our findings are not in agreement with the hypothesis that exposure to novel agents in relapsed/refractory settings leads to resistant clone selection under stress. The pattern of relapse in standard risk myeloma remains same across lines of therapy. Excellent response rates are observed with novel agents at relapse therefore delaying transplant appears reasonable in standard risk. High-risk myeloma represents a unique subset where patients experience early/aggressive relapse indicating that current therapy offers little modification of kinetics or natural history of disease. Changing treatment paradigm based on disease risk and response appears pragmatic. Myeloma is the disease of elderly with plethora at hand, its time to individualize.
Disclosures
No relevant conflicts of interest to declare.